Health Resources in Action’s Asthma Regional Council (ARC) established the New England Asthma Innovation Collaborative (NEAIC) in 2012 with a Center for Medicare and Medicaid Innovation (the Innovation Center) Health Care Innovation Award. NEAIC’s goal is to improve asthma outcomes, quality of care, and health care costs, especially for Medicaid and State Children’s Health Insurance Program (CHIP)-enrolled children, by advancing asthma home visits and sustainable payment systems across four New England states: Connecticut, Massachusetts, Rhode Island and Vermont. This goal supports the Innovation Center's aim to achieve better care for patients, better health for communities, and lower costs through improvements to the health care system. NEAIC achieves this goal through asthma self-management education; home environmental assessments, including minor-to-moderate environmental intervention supplies to mitigate asthma triggers; and use of nonphysician providers shown to be cost-effective deliverers of this level of care, particularly community health workers (CHWs) and certified asthma educators (AE-Cs).
During NEAIC’s 3 years of Innovation Center funding, providers utilized CHWs and AE-Cs to provide evidence-based home visit assessments and interventions. The target population was pediatric patients (ages 2–17) with poorly controlled or uncontrolled asthma symptoms who had a history of using expensive urgent care, with a focus on high-cost Medicaid and CHIP patients. Patients were enrolled in the intervention for an average of 6 to 8 weeks, with followup at 6 and 12 months after the first home visit. Medicaid payers provided patient claims and encounter data to monitor costs and outcomes for their patient populations, and some will consider new reimbursement policies should the interventions demonstrate positive health and cost outcomes.
Broadly, NEAIC focuses on four components: (1) workforce development, (2) rapid service delivery expansion, (3) committed Medicaid payers, and (4) a Payer and Provider Learners Community. Each component builds in continuous quality improvement measures through rigorous data collection/analysis, strong partnerships, and commitments from interested payers and policymakers.
In support of a well-trained workforce, NEAIC has provided scholarships for individuals to attend an asthma training institute to increase the number of AE-Cs; they also sponsored core training (a 48-hour course) and asthma home visiting training (a 24-hour course) for CHWs. Both asthma educators and CHWs are considered qualified and cost-effective providers. NEAIC also explored payers’ attitudes, knowledge and beliefs about both asthma home visits and CHWs. These conversations led to recommendations for innovative CHW asthma-credentialing programs that payers and provider practices across New England have requested and can benefit from. These combined efforts should contribute to higher-quality and culturally competent care, and NEAIC believes that the demonstrated cost-effective outcomes will help support innovative Medicaid reimbursement.
NEAIC experienced rapid service delivery expansion and provided asthma home visits to 1,145 high-risk children with asthma in its four-state service area during its 3 years of Innovation Center funding. Self-reported data and observations during home interventions show improvements to several intermediate factors, including exposure to environmental triggers, which may explain the improved asthma control and reported decreases in the use of health care services. Findings point to improved quality of life for asthma patients and their caregivers, including a nearly 50-percent reduction in the number of days patients missed school because of asthma and a more than 60-percent reduction in their caregivers’ missed work days.
Since its inception, NEAIC has engaged Medicaid payers as partners to provide claims data, participate in regional meetings, and consider financing and policy changes should the service model results achieve the Innovation Center’s aims.
The Payer and Provider Learners Community exists to rapidly disseminate demonstrated improvements to the quality and cost of asthma care, share viable reimbursement systems developed, successfully incorporate CHWs into the asthma care team, and disseminate best practices across New England. The Learners Community builds on ARC’s existing networks and partnerships across the region to increase awareness about these successful models, with the goal of broader adoption across New England.
Through these four components, NEAIC establishes and promotes CHWs as strong health care delivery partners who address environmental conditions as part of the disease management program—with reimbursement by payers—making this an innovative model for broad dissemination and potential replication across the nation.
NEAIC’s Partners
Clinical Providers
- Boston Children’s Hospital (Boston, MA)
- Baystate Children’s Hospital (Springfield, MA)
- Boston Medical Center (Boston, MA)
- Children’s Medical Group (Hamden, CT)
- Middlesex Hospital (Middletown, CT)
- Rhode Island Hospital/Hasbro Children’s Hospital (Providence, RI)
- Rutland Regional Medical Center (Rutland, VT)
- St. Joseph’s Health Clinic (Providence, RI)
- Thundermist (Woonsocket, RI)
Workforce Development Partners
- Central Massachusetts Area Health Education Center, Outreach Worker Training Institute (Worcester, MA)
- American Lung Association of the Northeast (Waltham, MA)
- Boston Public Health Commission, Community Health Education Center (Boston, MA)
- Massachusetts Association of Community Health Workers (Worcester, MA)
Medicaid Payers
- BMC HealthNet Plan (Boston, MA)
- Department of Vermont Health Access (VT State Medicaid)
- Connecticut Department of Social Services (CT State Medicaid)
- Health New England (Springfield, MA)
- MassHealth (MA State Medicaid)
- Neighborhood Health Plan of Massachusetts (Boston, MA)
- Neighborhood Health Plan of Rhode Island (Providence, RI)
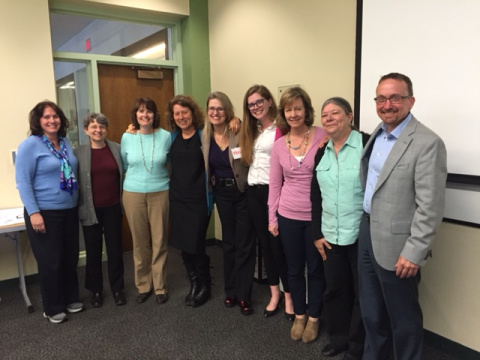
Marie Gilmond (Rutland Regional Medical Center, VT), Susan Sommer (Boston Children’s Hospital, MA), Veronica Mansfield (Middlesex Hospital, CT), Stacey Chacker (Health Resources in Action), Megan Sandel (Boston Medical Center, MA), Annie Rushman (Health Resources in Action), Elizabeth McQuaid (Hasbro Children’s Hospital, RI), June Tourangeau (St. Joseph Health Center, RI), Michael Corjulo (Children’s Medical Group, CT). Missing from this picture is Matthew Sadof (Baystate Medical Center, MA), Donna Needham (Thundermist Health Center, RI) and Heather Nelson (Health Resources in Action)