Mobile Care Chicago

Mobile Care Chicago is a not-for-profit organization that uses mobile medical clinics to assist children currently unable to access necessary specialty care for a chronic condition. For 19 years, Mobile Care Chicago has used partnerships with local schools to provide a convenient and trusted location for local children who have complex needs but whose parents may not have the time, transportation or work flexibility to access more distant brick-and-mortar clinics. Mobile Care Chicago currently operates two Asthma Vans for children with severe asthma and/or allergies, a Dental Van for children who need oral surgery, and a Portable Dental Clinic that can be set up inside of schools to make referrals to the Dental Van. In total, Mobile Care Chicago’s mobile clinics serve roughly 8,000 patients per year, seeing the vast majority multiple times per year.
Research suggests that in lower income Chicago neighborhoods, such as Humboldt Park and the South Shore, more than 25% of children have asthma. Chicago has the second-most asthma fatalities of all cities in the United States, according to the Asthma and Allergy Foundation of America. Most fatalities happen in Cook County neighborhoods where asthma is not well-controlled because of lack of available medical care. The Illinois Department of Public Health estimates that 76.5% of children with asthma in Illinois qualify as “not well-controlled, with the vast majority of cases reported in low-income areas.”
Asthma Vans go directly into lower income communities where specialty care access is an issue. The Asthma Vans then provide ongoing medical support to children with asthma, with a focus on adopting the medical care of its patients from their first appointment until the child turns 19 or graduates from high school. The average patient currently stays with their Asthma Van for more than 7 years. Mobile Care Chicago has screened more than 125,000 children for asthma in its 19-year history and provided comprehensive asthma care to more than 12,000 vulnerable children through more than 44,000 patient visits.
In recent years, Mobile Care Chicago has focused on high-intensity interventions for children with the most severe asthma/allergy conditions, including some children who had been cycling through local emergency departments more than 50 times per year. Through a team of nurse practitioners, allergists and community health workers, the Asthma Vans provide a series of home environment assessments, direct medical treatment and therapy, telemedicine and telehealth support for families, on-going education, and a 24-hour hotline staffed by the nurse practitioner team. The 3-year pilot of this high-intensity asthma control method reduced pediatric asthma emergency room visit rates by 84% in one Chicago hospital that previously had one of the highest rates of asthma admittances.
Patients assisted through the Asthma Vans have seen a more than a 50% decrease in school absenteeism and emergency department visits. Last year, only 6% of Asthma Van patients used an emergency room, versus 55% in the year prior to enrollment. The reduction in hospitalization rate alone (19% to 2% for Mobile Care Chicago patients) has saved the local health care system at least $156 million during the past 13 years. In addition, the Illinois Department of Public Health estimates that uncontrolled asthma costs the state of Illinois $15,155 per individual. By contrast, Mobile Care Chicago spent an average of $836 on each patient in the last fiscal year. This represents a 94% savings for each patient whose asthma is controlled.
Mobile Care Chicago’s early intervention screenings and mobile medical care delivery in hard-to-access and low-income communities has encouraged action and change in the surrounding Chicago communities, bringing asthma relief for thousands of children and peace of mind for parents.
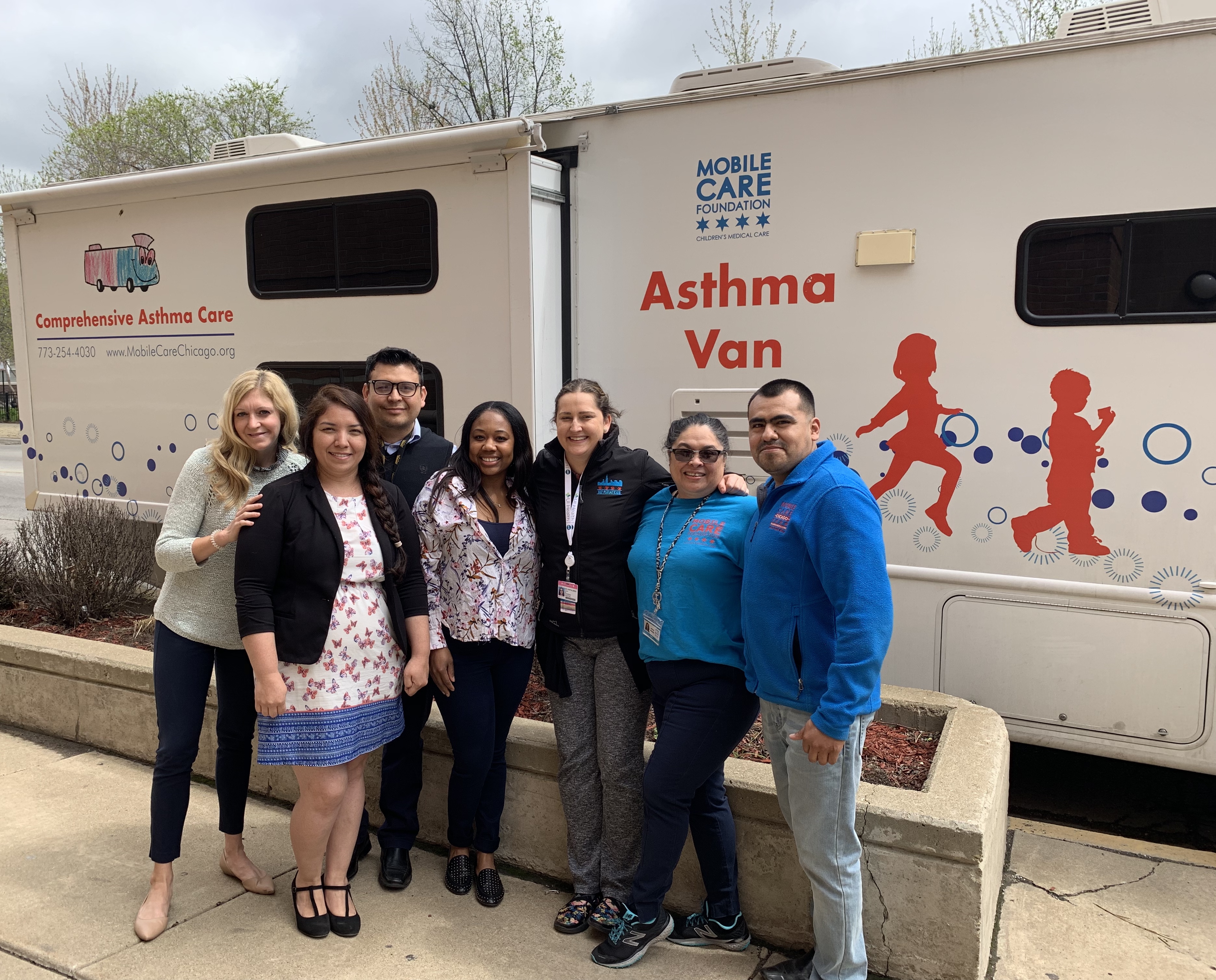
From left to right: Amy Bain, CPNP; Jorge Mendoza (van driver); Elizabeth Lemus (Asthma Program Manager); Kamari Thompson (Community Health Worker); Dr. Andrea Pappalardo (Allergist); Sandra Morales (MA); Raul Hernandez (van driver)




